What we do
Our turnkey, patent pending technology platform enables:
- Connection to any enrollment platform, carrier, benefits administrator or database system
- Full circle enrollment data consumption, interrogation, decisioning, and response processing from >300 sources
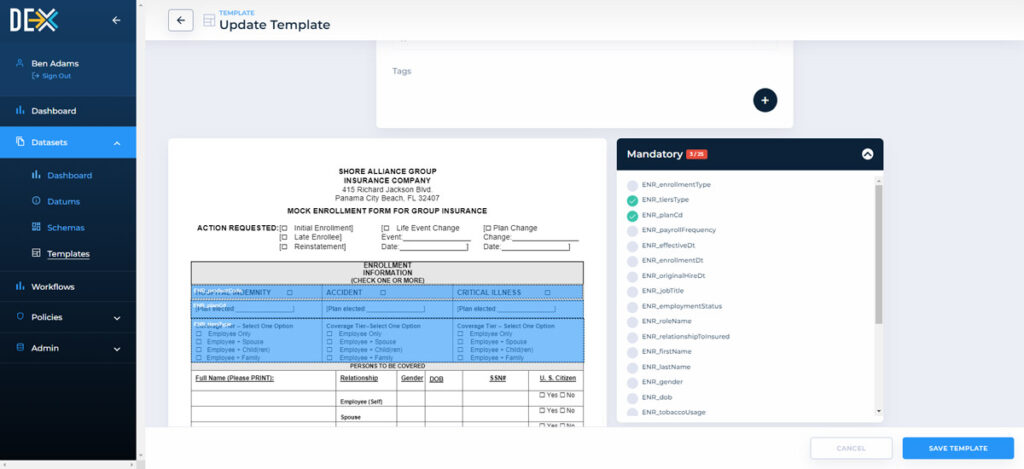
- API / EDI / and even paper (we auto convert handwritten entries to digital data)
- Processing in ANY format (e.g. JSON, XML, csv, delimited, etc.)
- LIMRA LDEx ‘Easy’ button (for auto conversion to or from LIMRA LDEX format)
- Enrollment, Data Interrogation, Instant Decisioning, Policy/Certificate Issuance
- EOI, Case Setup Details, Issuance Status, Quoting and Claims DB updates
Our Solutions
- Eliminate the need to convert legacy systems (Policy Admin., Claims, Billing, Commission)
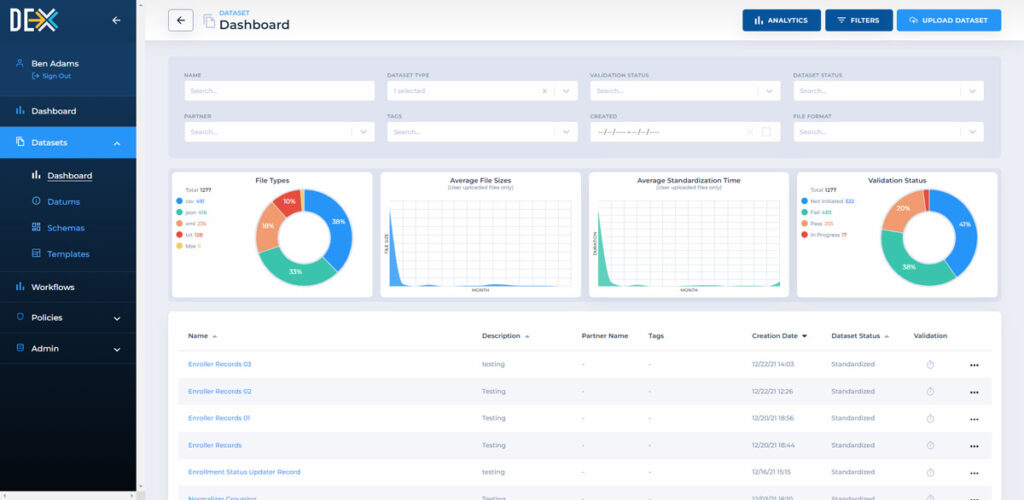
- Provide Dashboards, KPIs and Business Insights for Broker & Enrollment Partners and even Employer Groups
- Utilize full versioning and end-to-end data auditability across the ecosystem
- Provide seamless partner onboarding and integration
- Automatically notify designated stakeholders of issuance disposition status and provides in depth dashboarding and tracking
- Are offered as either SaaS-based or Hosted Solutions
Shore solutions enable client growth
New business growth
Greatly expands distribution reach to brokers with turnkey solutions.
Expense reduction
Reduce/eliminate current expenses for data management, back office processing, and future enrollment platform investment.
Expanded business model
Get access to key legislative and regulatory engagement, harness affinity and industry relationships, and more.
Market innovation
Capitalize on universal engagement and ease of use through an API hub, HSA compatibility and data standards.
How DEX® helps
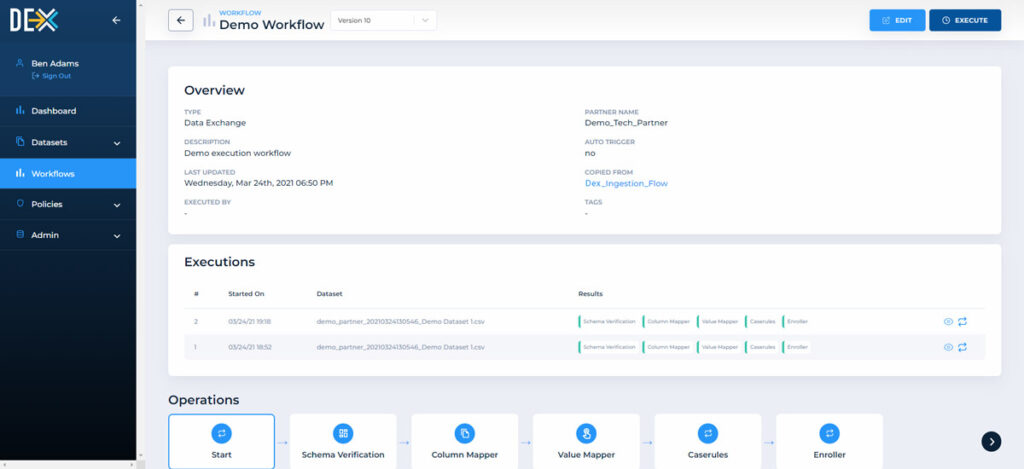
- Receive from any enrollment platform or benefits admin system via APIs or EDI datasets
- Inbound data is translated within DEX® and maps to appropriate data fields in any legacy system
- Schemas are mapped only once for each partner (not for every file or dataset)
- Eliminates the need to convert legacy systems (Policy Admin., Claims, Billing, Commission)
- DEX® interrogates enrollment data against product and case rules, validating records in good order (IGO) for immediate processing while pending records not passing one or more validations (NIGO)
- One time schema mapping creates turnkey connectivity to any carrier
- Send data to any carrier or Database System via APIs or EDI datasets
- Enrollment data is translated within DEX® and maps to appropriate data fields in the carrier’s legacy system
- DEX® passes real time response from a carrier policy admin system complete with record level detail issuance confirmation and coverage details
- Provides Case Setup details automatically
DEX® enabled enrollment processing shifts end to end enrollment from weeks to minutes and can provide Broker – level Dashboards spotlighting trends in:
- Participation rates, conversion rates, retention
- Persistency rates and average premium by coverage
- Instant updates on coverage issuance status and record level detail
DEX® enables bulk updates to legacy database systems with no need to ever convert legacy systems
- Create bulk claims database updates
- Update policy admin systems in a single step
- Translate data from any format into any other format via APIs, EDI/Datasets, or even via paper-based sources
- Support business processes with data interrogation capabilities
- Generate system-wide reporting and dashboards